Sterilization & Disinfection
Definition
According to the CDC (Centers for Disease Control and Prevention), “Sterilization means the use of a physical or chemical procedure to destroy all microbial life, including highly resistant bacterial endospores.”
Sterilization is an absolute term, i.e. the article must be sterile meaning the absence of all microorganisms.
Although the chemical or physical process used to destroy all pathogenic microorganisms
including spores is not absolute, when all parameters of the sterilization process have been met, instruments, supplies and equipment are thought to be sterile.
Sterilization is categorised into:
1. Heat Sterilization
2. Filtration
3. Radiation sterilization
4. Chemical sterilization
The common sterilization methods within each category:
| I. Heat Sterilization | |
| i. Dry Heat | i. Incineration |
| ii. Flaming | |
| iii. Hot Air Oven | |
| ii. Moist Heat | i. Temperature below 100OC |
| ii. Temperature at 100OC | |
| iii. Temperature above 100OC | |
| II. Filtration | |
| III. Chemical | i. Ethylene Oxide (EtO) |
| ii. Low Temperature Plasma Vapor | |
| iii. Glutaraldehyde | |
| iv. Formaldehyde | |
| v. Ethanol | |
| vi. Chlorine Dioxide | |
| vii. Ozone | |
| IV.Radiation | i.Gamma |
| ii. Electron Beam (E-Beam) | |
| iii.X-rays | |
| iv. UV rays |
Whatever method of sterilization is chosen, the procedure must be validated for each type of material, both with respect to the assurance of sterility and to ensure that no adverse change should take place.
Biological indicators are used to validate sterilization methods and sometimes for routine control of individual cycles. Periodic revalidation is recommended.
I. Heat Sterilization
i. Dry-heat sterilization
In dry-heat processes, the primary lethal process is considered to be oxidation of cell constituents. Dry-heat sterilization requires a higher temperature than moist heat and a longer exposure time.
Incineration
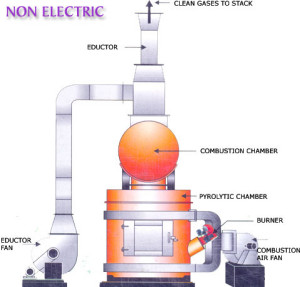 |
8700C – 9800C Complete burning to ashes Used for soiled dressings, animal carcasses, pathological material, disposables, non-reusable soiled bedding |
Flaming
Hot Air Oven
Holding temp & time: 1600C for 1 hr
Used for glassware, forceps, swabs, water impermeable oils, waxes & powders
Before placing in hot air oven
Dry glassware completely
Plug test tubes with cotton wool
Wrap glassware in Kraft papers
Don’t over load the oven.
Allow free circulation of air between the material.
The method is, therefore, more convenient for heat-stable, non-aqueous materials that cannot be sterilized by steam because of its deleterious effects or failure to penetrate.
Preparations to be sterilized by dry heat are filled in units that are either sealed or temporarily closed for sterilization. The entire content of each container is maintained in the oven for the time and at the temperature given in the table below. Other conditions may be necessary for different preparations to ensure the effective elimination of all undesirable microorganisms.
Temperature
(°C) Minimum sterilization time
(min)
160 60 mins
180 30 mins
Specific conditions of temperature and time for certain preparations are stated in individual monographs.
The oven should normally be equipped with a forced air system to ensure even distribution of heat throughout all the materials processed. This should be controlled by monitoring the temperature. Containers that have been temporarily closed during the sterilization procedure are sealed after sterilization using aseptic techniques to prevent microbial recontamination.
The bioindicator strain proposed for validation of the sterilization process is: spores of Bacillus subtilis (e.g. var. niger ATCC 9372) for which the D-value is 5-10 minutes at 160 °C using about 106 spores per indicator.
ii. Moist Heat
Moist heat – Temp below 1000C
Pasteurization
• 630C – 30 min (Holder method)
• 720C – 15-20 sec (Flash method)
• 1320C – 1 sec (Ultra high temp)
Vaccine baths – 600C – 60 min
• For vaccines of non-sporing bacteria
Water bath – 560C – 60 min – 3 days
• For serum / body fluids containing coagulable proteins
Inspissation – 80-850C – 30 min – 3 days
• For media containing egg or serum – LJ
Moist Heat – Temp at 1000C
Boiling – 1000C for 10 min.
Kills all vegetative bacteria.
Water should be soft, deionized or distilled.
2% sodium bicarbonate promotes the process.
Kills vegetative bacteria, hepatitis virus & some spores
Steaming (free steam) – 30-60 min in Arnold /Koch steamer
For heat labile media – DCA, TCBS
Tyndallisation (intermittent sterilization) – 1000C, 30 min, 3 days. On Ist day all vegetative bacteria are killed. On IInd & IIIrd day spores that germinate are killed.
Nutrient media & media containing sugars or gelatin.
 |
 |
 |
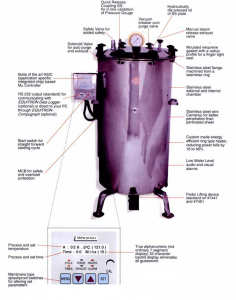
| Portable Autoclave | Vertical Autoclave | Horizontal Autoclave |
Moist heat – Temperature above 100OC
Autoclave (steam under pressure) – 1210C, 15-20 min, 15 lbs
Used for rubber articles, dressings, sharp instruments, infectious medical waste, culture media
Sterilization control
Browne’s tube (red-green), Bowie & Dick tape (white-brown)
106 spore of Bacillus stearothermophilus. Incubate at 550C for 5 days
Steam autoclave is the oldest, safest, and most cost effective method of sterilization. The steam reaches 121-148OC (250-300OF) in the pressure chamber at 15 P.S.I. The sterilization period is dependent on the temperature and size of load and can range from 10-60 minutes. This method is not well suited for heat sensitive materials and instruments.
The common types of steam sterilization cycles are gravity-displacement, which removes air from the chamber by gravity displacement as steam-entering chamber exerts pressure on air; and the pre-vacuum cycle, which removes air by a vacuum pump while steam is simultaneously injected into the chamber.
Exposure of microorganisms to saturated steam under pressure in an autoclave achieves their destruction by the irreversible denaturation of enzymes and structural proteins. The temperature at which denaturation occurs varies inversely with the amount of water present. Sterilization in saturated steam thus requires precise control of time, temperature, and pressure. As displacement of the air by steam is unlikely to be readily achieved, the air should be evacuated from the autoclave before admission of steam. This method should be used whenever possible for aqueous preparations and for surgical dressings and medical devices.
In the steam autoclave process, microorganisms are killed by heat, and this is accelerated by the addition of moisture. Steam by itself is not sufficient for sterilization, and pressure that is greater than atmospheric is needed to increase the temperature of steam for thermal destruction of microbial life.
Steam, for a specified time at required temperature, must penetrate every fiber and reach every surface of items to be sterilized. When steam enters the sterilization chamber under pressure;
It condenses upon contact with cold items.
This condensation frees heat, simultaneously heating and wetting all items in the load, thus providing heat and moisture.
Any living thing will be killed when exposed to saturated steam at 120OC (250OF) longer than 15 minutes. As temperature is increased, time may be decreased.
The recommendations for sterilization in an autoclave are 20 minutes at 121-124 °C (200 kPa)/15lb pressure. The temperature should be used to control and monitor the process; the pressure is mainly used to obtain the required steam temperature.
Minimum sterilization time should be measured from the moment when all the materials to be sterilized have reached the required temperature throughout. Monitoring the physical conditions within the autoclave during sterilization is essential. To provide the required information, temperature-monitoring probes should be inserted into representative containers, with additional probes placed in the load at the potentially coolest parts of the loaded chamber (as established in the course of the validation programme). Each cycle should be recorded on a time-temperature chart or by other suitable means.
Application:
1. Steam autoclave is used mostly for surgical instruments & sharp instruments.
2. In certain cases, glass, porcelain or metal articles, liquids in vented containers are sterilized at 121 – 124 °C for 20 minutes.
3. Fats and oils may be sterilized at 121 °C for 2 hours but, whenever possible, should be sterilized by dry heat.
4. Used for rubber articles, dressings, infectious medical waste, culture media
In certain cases (e.g. thermolabile substances), sterilization may be carried out at temperatures below 121 °C, provided that the chosen combination of time and temperature has been validated. Lower temperatures offer a different level of sterilization; if this is evaluated in combination with the known microbial burden of the material before sterilization, the lower temperatures may be satisfactory. Specific conditions of temperature and time for certain preparations are stated in individual monographs.
The bioindicator strain proposed for validation of this sterilization process is: spores of Bacillus stearothermophilus (e.g. ATCC 7953) for which the D-value (i.e. 90% reduction of the microbial population) is 1.5-2 minutes at 121 °C, using about 106 spores per indicator.

